Vaccines have become one the fastest growing pharmaceutical markets in the world, with major investments in research and development, manufacturing and more. The global human vaccine market has a forecasted potential market growth of USD 18.52 billion between 2021-2025.
This development is in line with the increasing frequency of infectious diseases, innovative technology used in vaccine development, increased funding from both government and international organisations, and increasing awareness towards preventive care.
As a powerful public health tool, vaccines save millions of lives each year. However, millions of dollars in vaccine doses are lost when vaccines lose their efficacy and have to be disposed.
Proper storage is important for the effectiveness of vaccination programmes, and medical staff must be vigilant when handling and dispensing vaccines.
In that way, unnecessary expenses can be avoided for the medical facility and more people can be helped by allowing them access to the vaccines they need.
The storage and handling guidelines for each vaccine differs. To ensure successful vaccine storage and avoid catastrophic vaccine loss, medical facilities should follow these dos and donts:
1. Effective Temperature Maintenance
Most vaccines require low temperatures during transportation and storage in order to remain effective. When vaccines need to be sent long distances to countries and regions where environmental temperature are pretty high, it is important to have suitable cold chain arrangements in place.
Cold chain practices tend to prioritise the protection of vaccines from heat damage. However, another issue arises which is often overlooked. Vaccines which should be optimally stored between 2°C and 8°C, may be at risk of accidental freezing instead.
Hence, the maintenance of accurate and uniform temperatures is significantly important. Any deviation above or below the optimal temperature range will cause a vaccine to lose its efficacy and result in massive losses for the medical facility.
Medical workers and employees should be educated on the proper storage and handling of various vaccines if they routinely handle vaccines.
2. Observing Expiration Dates
When unloading a shipment of vaccines, some batches may have different expiration dates. These dictate which vaccines should be used first as vaccines lose their efficacy after the expiry date. In fact, vaccines even a day over their expiration date should not be used.
Giving a patient an expired vaccine means that the protection the vaccine is supposed to provide is far reduced and more time and effort will be needed to revaccinate besides the traumatic experience it can cause to younger patients.
As a standard practice, medical workers or employees should check expiration dates of all vaccines once received at a medical facility. By doing so, vaccines with the earliest expiration date can be identified.
These should be stored at the front of the vaccine storage unit and be highly accessible. Vaccines with later expiration dates can be rotated to the front of the unit as the batches are finished. Regular checks should also be performed on the vaccine storage unit in order to check for any expired vaccines.
3. Storing Vaccines Appropriately
Drugs are typically unpacked after receiving them from manufacturers before storing at designated areas within a medical facility.
Vaccines however, may come with special packaging to preserve the contents. Hence, it is best to keep them in their original packaging.
As a best practice, adopt the CDC toolkit guidelines for ensuring the proper storage of vaccines and assist in creating practice-specific protocols.
The guidelines have been updated with the details on storage and handling best practices for COVID-19 vaccines to be in line with the current pandemic.
4. Choosing the Correct Storage Unit
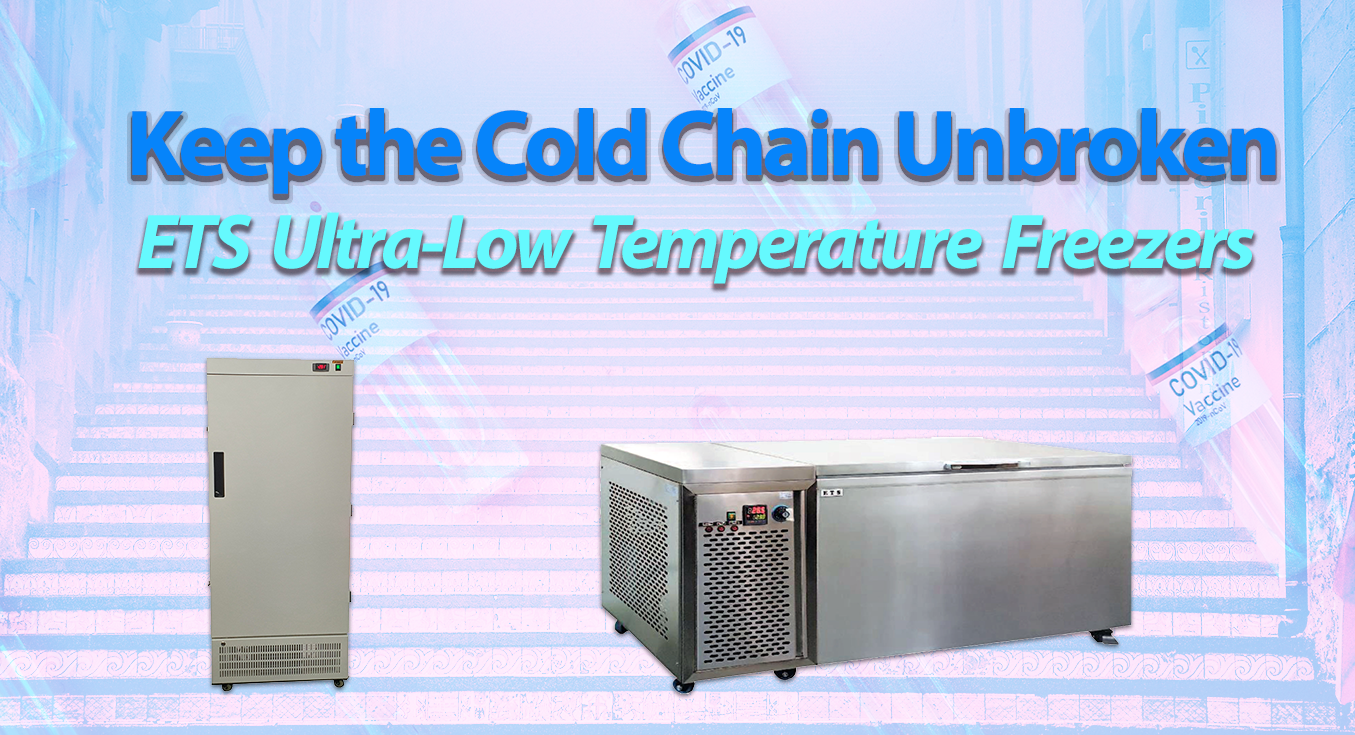
Different vaccines have different temperature requirements, so choosing the right cold storage unit is highly critical. There are pharmaceutical-grade or purpose-built cold storage units that can effectively maintain the optimal temperature range.
For example, refrigerators designed for vaccine storage operate at temperatures between 2°C and 8°C, freezers between -50°C and +5°C, while Ultra-Low Temperature freezers (ULTs) can reach temperatures as low as -86°C.
Cold storage units require good ventilation around the unit, and should be kept in a room with a standard room temperature of between 20°C and 25°C.
In addition, quite a bit of space is required for vaccine storage, and it should not completely fill up the cold storage unit. There should be enough space in between the vaccines to facilitate air circulation inside the cold storage unit, which helps to maintain an uniform temperature and quicker temperature recovery after door openings.
5. Monitoring Cold Storage Units
If the door on a cold storage unit is left open inadvertantly, or failed to seal properly, then the internal temperature of the unit will fluctuate.
When a slow leak happens through a failed seal, it would take some hours before triggering the fridge or freezer’s alarm, by which time, vaccines stored in the unit may already be affected by the temperature fluctuation.
An accurate and reliable temperature monitoring system is vital to protect the integrity of the vaccines and other temperature-sensitive drugs stored inside a cold storage unit.
Whether using a digital data logger (DDL) or real-time monitoring service, the medical facility must consistently monitor the temperatures inside the cold storage unit, as well as the environmental conditions.
This is to ensure efficient operations of the unit, detect any significant temperature change that could affect the unit’s contents and inform persons-in-charge in a timely manner.
5. Maintenance is Key
Vaccine cold storage units must be maintained regularly to protect their contents and the safety of patients.
Regular preventive maintenance would include the calibration testing of temperature monitoring devices (TMDs) after purchase and an annual checkup according to manufacturer recommendations.
On the other hand, routine maintenance should be practiced by employees of the medical facility, which includes testing door seals and hinges, cleaning the interior to prevent bacterial and fungal growth, and observing the frost buildup of the cold storage unit. If too much frost builds up, it can interfere with air circulation and door seals.
Environmental factors can also affect cold storage units, so it’s vital to monitor conditions in the room where cold storage units are placed. Areas with seasonal climates may see room temperatures fluctuate as well, so adjustments need to be made accordingly.
6. Prepare for the Unexpected
The unexpected can happen at any time.
If your medical facility loses power suddenly, the first thing to be affected would be your cold storage units storing valuable vaccines. Most medical facilities keep backup generators on hand to keep their cold storage units running in this kind of situation.
Another common emergency is the accidental unplugging of cold storage units by employees. It would generally take some time before the unit is plugged in again, by which time its contents would already be under temperature deviation and its shelf life affected.
Therefore, employees and cleaning staff should be made to understand that cold storage units should never be unplugged.
In addition, a facility with cold storage units should keep an emergency protocol in place. This protocol should include alternative storage methods, such as backup storage units in the event of unit failure, or what to do in the event of massive power outages. To avoid data gaps and missed alerts, it is also recommended to have monitoring systems with 4G connectivity.
Conclusion
Following best practices in order to ensure proper vaccine storage is not just beneficial to the medical facility but also the patients who will receive those vaccines. Proper education of employees and appropriate quality control measures will ensure less chances of costly losses and potential revaccination programmes.
LOOKING FOR A MEDICAL-GRADE COLD STORAGE UNIT?
ETS Pharmaceutical Refrigerators and Freezers are designed and fabricated to meet the demanding requirements of scientific and laboratory applications. These refrigerators and freezers provide a complete and integrated solution for storage of pharmaceuticals, medicines, biological products and reagents, vaccines, etc.
To know more, check out our Pharmarceutical/Laboratory refrigerators and Pharmaceutical Freezers.
Drop us a line if you have questions.